Interdisciplinary Collaboration in Wound, Ostomy, and Continence (WOC) Care: A Guide for Nurses, OTs, and PTs
In the evolving landscape of healthcare, wound, ostomy, and continence (WOC) care stands out as a field where teamwork isn’t just beneficial—it’s essential. As patient needs become more complex, involving conditions like pressure injuries, ostomy management, and incontinence, the collaboration between nurses, occupational therapists (OTs), and physical therapists (PTs) can significantly improve outcomes. This blog explores the critical role of interdisciplinary collaboration in WOC education and practice, drawing on real-world insights to highlight why integrating these professions leads to better patient care. Whether you’re a seasoned nurse specializing in wound care or a therapist looking to expand your skills, understanding this synergy is key to advancing your career.
Why Interdisciplinary Collaboration Matters in WOC Care
WOC care encompasses a wide range of challenges, from preventing skin breakdowns in immobile patients to supporting individuals with ostomies in daily living. Traditionally, nurses have led the charge in this area, often certified as Wound, Ostomy, and Continence Nurses (CWOCNs) through programs requiring a baccalaureate degree and specialized training. However, the complexity of these issues demands input from multiple disciplines. For instance, a multidisciplinary approach can prevent complications like pressure ulcers by combining nursing assessments with therapeutic interventions from OTs and PTs.
Research underscores the value of this collaboration. A study evaluating collaborative management between orthopedic surgeons and WOC nurses found improved patient outcomes in postoperative care, including reduced infection rates and faster healing. Similarly, in pressure management, an interdisciplinary model involving therapists and wound care nurses has been shown to enhance prevention and assessment strategies. These examples illustrate how pooling expertise—from nursing’s focus on wound assessment to therapy’s emphasis on mobility and function—creates a holistic care plan that addresses both medical and functional needs.
In fact, a cross-sectional study in China highlighted factors influencing interprofessional collaboration among WOC nurses, emphasizing communication, shared goals, and role clarity as key to success. When applied to teams including OTs and PTs, this collaboration reduces hospital readmissions and improves quality of life for patients with chronic conditions.
The Unique Roles of Nurses, OTs, and PTs in WOC Collaboration
Each profession brings distinct strengths to WOC care, making interdisciplinary teams more effective than siloed approaches.
- Nurses: As the frontline in WOC, nurses handle direct wound care, ostomy education, and continence management. They perform assessments, apply dressings, and educate patients on self-care. In collaborative settings, nurses act as coordinators, ensuring that therapeutic plans align with medical protocols. For example, in a rehabilitation team, nurses might work with therapists to develop admission assessments that incorporate WOC-specific tools.
- Occupational Therapists (OTs): OTs focus on how WOC issues impact daily activities. They adapt environments for ostomy patients, recommend assistive devices for continence, and train individuals in self-management techniques. In interdisciplinary teams, OTs bridge the gap between medical treatment and functional independence, such as modifying bathrooms to prevent skin irritation from poor positioning.
- Physical Therapists (PTs): PTs emphasize mobility and strength, crucial for preventing pressure injuries and aiding recovery post-ostomy surgery. They design exercise programs that promote continence through pelvic floor strengthening and work with nurses to integrate wound-safe movement strategies. A multidisciplinary wound care team often includes PTs alongside nurses and surgeons to address mobility-related risks.
When these roles intersect, this is where the magic happens! Consider a patient with a colostomy facing mobility challenges: A nurse might manage the stoma site, an OT could adapt clothing for easier access, and a PT could prescribe exercises to build core strength—all coordinated for optimal results. Organizations like the Wound, Ostomy, and Continence Nurses Society (WOCN) advocate for such integrated practices, recognizing WOC nurses’ pivotal role in multidisciplinary teams.
Real-World Benefits and Challenges of Collaboration
The advantages of interdisciplinary collaboration in WOC are well-documented. Teams that include nurses, OTs, and PTs report better patient satisfaction, fewer complications, and cost savings for healthcare facilities. For professionals, it means enhanced learning opportunities, such as cross-training in wound staging or therapeutic techniques, leading to certifications and career growth.
However, challenges exist, including communication barriers and differing professional cultures. Overcoming these requires education and shared platforms—like conferences—where professionals can learn together. A review of WOC nursing development notes that fostering collaboration through specialized training is vital for advancing the field.
Elevate Your WOC Skills Through Collaborative Education
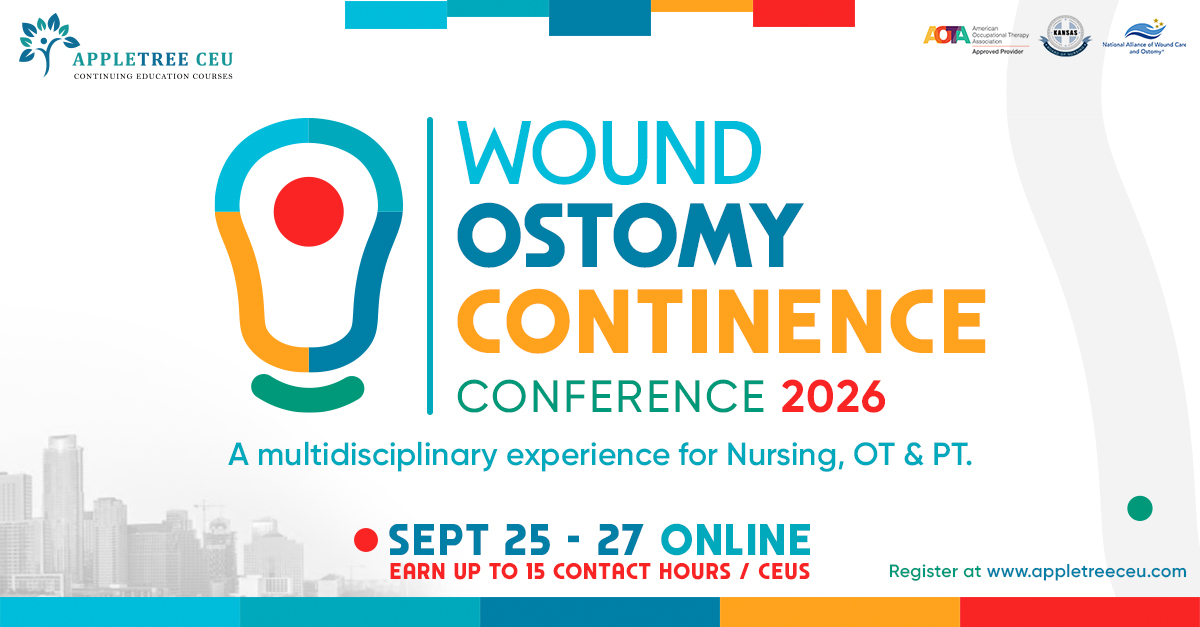
To truly harness the power of interdisciplinary collaboration, ongoing education is key. Most conferences on these topics focus solely on the role of one discipline, which in my opinion is not the best way to achieve the best patient outcomes or bring teams together. That’s why our team has created an online WOC Conference with a true focus on interdisciplinary collaboration. Scheduled for September 2026, this virtual event is designed specifically for nurses, OTs, and PTs, offering sessions that emphasize teamwork in wound, ostomy, and continence care.
Our conference features expert-led workshops on topics like bowel and bladder management, ostomy management, wound care and multidisciplinary continence strategies. You’ll hear from leaders in nursing, occupational therapy, and physical therapy, gaining practical insights to apply in your practice.
Whether you’re seeking to earn contact hours, network with peers, or deepen your understanding of interdisciplinary approaches, this conference is your gateway to excellence in WOC care.
Ready to Collaborate and Advance Your Career?
Don’t miss out on this opportunity to transform your approach to WOC through interdisciplinary collaboration. To learn more and register, you can do so by clicking here – AppleTree CEU’s Online WOC Conference 2026 . Join a community dedicated to innovative, patient-centered care. Spots are limited—secure yours now and take the next step in your professional journey!